Return guest Dr. Paul Saladino is a board-certified psychiatrist and likewise board licensed in nutrition. He wrote “The Carnivore Code, ” which just came out in an updated second volume. In this interview, he discusses the impact metabolic health has on COVID-1 9 outcomes.
He’s done a elegant place illustrating the science that supports the natural lifestyle programmes that optimize our immune systems to defeat not only COVID-1 9, but likewise most other infectious agents.
“The psychiatry was a jump-off point for thinking about how immune function and metabolic health alters mental health, ” he says. “I rapidly realized that everything in the body was connected and I couldn’t time focus on the brain without focusing on the rest of the body, and that has led us to where we are today.
I think that as we are faced with coronavirus, it’s a remember of the metabolic health and how critical that is. I think so much of the media focus right now is on the next drug or the coming vaccine … but all of those strategies kind of miss the point.[ They’re] simply Band-Aids …
No drug is going to protect us from the next infectious diseases and the next illnes. And one of the things that we’re going to talk about today, which is so eerie, more divulging, is all of this data suggesting that coronavirus susceptibility is intimately connected with metabolic health.”
Immunometabolism Is an Important Field of Medicine
We’ve long was well known that metabolic health is crucial for robust immune function. Saladino conceives immunometabolism — the relationships between metabolism, metabolic health and the immune arrangement — is readily one of the largest part, if not the most important, subject in emerging medicine.
One of the classic varies that we see associated with insulin resistance, obesity and metabolic syndrome is overactivation of the innate immune organization, with decrease activity in the adaptive immune system.
Saladino reviews NHANES data1 from 2009 to 2016, which expose 87.8% of Americans are metabolically unhealthy, based on five constants. That data is over four years old now, so the figure is clearly greater than 90% of the population today.
That planneds virtually everyone is at risk for Type 2 diabetes and all the chronic diseases associated with insulin resistance, which passed the scope from cancer to Alzheimer’s.
“[ NHANES] use criteria that we use to define metabolic ailment, ” Saladino clarifies. “They use a waist circumference of less than 102 or 88 centimeters for men and women respectively, a fasting glucose of less than 100 milligrams per deciliter, haemoglobin A1c of less than 5.7, a systolic blood pressure less than 120, a diastolic blood pressure little than 80, and triglycerides less than 150, in addition to an HDL of greater than 40 for both men and 50 for women, as criteria for metabolic health.
What they found — and this is really the point that is so striking — is that merely 12.2% of parties converge that criteria. That implies 87.8% of people are metabolically unhealthy or have at least one of these metrics that suggests that they may have some degree of metabolic unhealth.”
Similarly, data from the U.S. Centre for Disease Control and Prevention shows that as of 2016, 39.8% of adults over the age of 20 were obese. When you include those who are overweight, that percentage soars to 71%, and excess force generally correlates with metabolic dysfunction and diminished health.
“Now, it’s not so much better an arraignment on our population; it’s an show, it’s a real call-to-arms to say,’ This is what we should be talking about, ’ and it’s a real jumping-off point for discussions about how metabolic unhealth has repeatedly been connected with worse outcomes,[ be it] COVID-1 9, MERS or seasonal influenza. It’s a huge piece of it, and I haven’t truly interpreted much media coverage of this at all.”
Insulin Resistance Is a Modern Plague
Indeed, while the media reports that the comorbidities include obesity, diabetes, age and being of color, they don’t discuss the underlying questions, which are vitamin D insufficiency and insulin defiance. As noted by Saladino 😛 TAGEND
“Insulin resistance underlies many of those comorbidities, and I’ll show data to suggest that as we age, more of the population becomes insulin-resistant, probably because we become a little less resilient to nutrient inadequacy and we become a little more sensitive to the lifestyle causes that move us insulin resistant in the first place.
With aging, we investigate a direct linkage with insulin defiance. But the immune settlement, the insulin fight that comes with aging, is not inevitable. It’s an assumption, because 88% of the population are metabolically unhealthy.
The narrative here is very important because if we can escape the immunologic sort of dysfunction and insulin fight that so often accompanies aging, then we can totally deepen our lifestyle.”
Metabolic Age Is More Important Than Biological Age
Saladino discusses the results of a Nature Medicine study2 be made available in 2019, which looked at immune age and metabolic age use high-dimensional longitudinal monitoring 😛 TAGEND
“You can look at multiple measures of immunologic age by looking at different diversifying proportions of immune cell subsets. This is all particularly esoteric and it seems complex, but the takeaway is that immune aging is associated with relative changes in different types of immune system response.
What’s very interesting is we encounter the same types of immune system response reforms reflected in people who have more severe coronavirus outcomes … One of the classic reforms associated with insulin resistance, obesity and metabolic syndrome — these are all synonyms — is overactivation of the innate immune plan, with decrease the actions of the adaptive immune system.
Characterized another way, we can look at the cytokines associated with different T-helper subsets. What we generally determine … is that sure-fire cytokines for T-helper 2 tend to predominate over T-helper 1, and you get changes in the way the innate and adaptive immune arrangements are responding to invaders. And that’s what we see in parties as they age.
That’s associated with activation of different inflammasomes, like the NLRP3 inflammasome, which is associated with that innate immune plan. The innate immune method is always initiated; it’s dendritic cadres, macrophages, natural killer cadres, neutrophils.
The adaptive immune organization is T cells and B cells. So basically, what we see in immunologic compromise, what we see in insulin resistance, is that the innate immune arrangement get overactivated at the expense of the adaptive immune system.
You might say,’ Oh, that’s good. One one of the purposes of the immune system is more activated.’ But what you have happening is that the adaptive immune arrangement isn’t able to be activated properly, and the solution of the swelling doesn’t happen in the way it should.”
So, the overarching principle is that it’s not your biological senility that matters so much better, but instead it’s your immune and metabolic age. The good bulletin is those are more malleable than we are led to believe. From that perspective, we can address COVID-1 9 in completely different ways.
“It’s a lot of fear-based messaging, saying,’ Here’s a brand-new spike of the virus.’’ It’s popping up now, it’s popping up there.’ But nobody’s genuinely talking about what you can do to change your susceptibility to this virus, ” Saladino says.
“What I was necessary to entitle people to understand is that this immunologic tolerance, this insulin resistance paradigm, has not been discussed at all despite the fact that there are tons of evidence that it’s actually, really important.”
Cytokines
Cytokines are small proteins exuded by cells in your innate and adaptive immune plans. They serve to regulate diverse performs in your immune response. Cytokines are released after cells into your circulation or directly into your tissues.
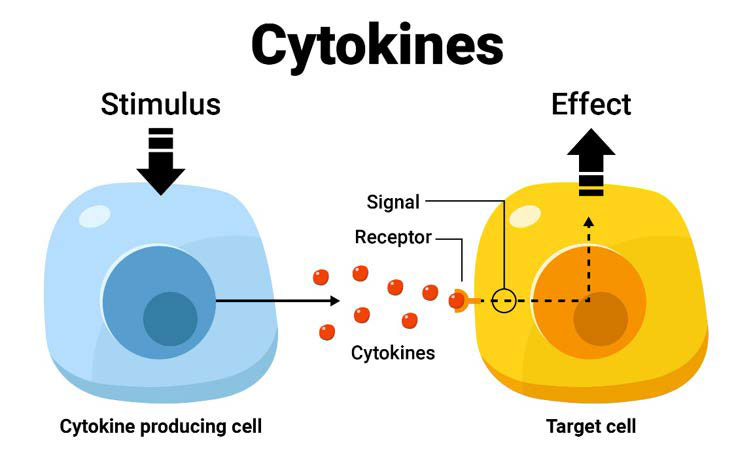
The cytokines unearth target immune cadres and treated with receptors on the target immune cells by fastening to them. The interaction prompts or energizes specific responses by the target cells.
In response to bacterial and viral infections such as COVID-1 9, your innate immune arrangement produces both proinflammatory and anti-inflammatory cytokines. 3 The inflammatory response represents a critical role in the clinical manifestations of COVID-1 9. SARS-CoV-2 initiations an immune response against the virus, which, if uncontrolled, may result in lung damage, functional disorder, and abbreviated lung faculty. 4,5, 6,7
The SARS-CoV-2 viral infection-related inflammation and the precede cytokine squall in severe cases performances a critical role in case existence. 8 The substantial and uncontrolled liberation of proinflammatory cytokines is called the cytokine whirlwind. Clinically, the cytokine gale frequently presents as systemic sorenes and variou organ disappointment. 9
Immunologic Tolerance Rises as Insulin Resistance Falls
One scientific article1 0 that speaks to this is “Association of Blood Glucose Control and Outcomes in Patients With COVID-1 9 and Pre-Existing Type 2 Diabetes, ” published in Cell Metabolism, June 2, 2020.
What it received was that when blood sugar is well-controlled and there’s less glycemic variability, beings done better when contracting COVID-1 9. When they have high levels of glycemic variability, which is indicative of insulin opposition, they fare much worse.
“So there’s actually no question at this point that glycemic variability, overall metabolic status, overall metabolic state are critical, ” Saladino says. The common mistake here is that you don’t wanted to that govern back exercising drugs. Your best bet is to get it back using natural lifestyle strategies.
Another paper1 1 that expresses the impact of insulin resistance on COVID-1 9 was published in Cardiovascular Diabetology, May 11, 2020. It determined you can use the triglyceride to glucose index( TyG index) as a reckon to prophesy the severity and death of COVID-1 9.
“Imagine that. There’s an association of the insulin resistance marker, the TyG index — this is fasting triglycerides, fasting glucose — with the seriousness and death of COVID-1 9.
This should be, in my view, mainstream word headlines, and the headlines ought to be,’ You is likely to be stronger against coronavirus. You can have a stronger immune system. You can abridge your risk of having a severe coronavirus outcome.’ But instead it’s largely fear, it’s’ Hide in your residences. What’s the next pharmaceutical that’s going to save us? ’ … Cardiovascular health is immune health. That is immunometabolism.
What you do to improve your heart health is also what you do to improve your immune health, is also what you do to improve your brain health, is also how you decrease your risk of Alzheimer’s, is also how you lessen the health risks of seasonal influenza and every other single infectious illness that you are able to all meeting for the rest of your life. It’s one thing; not 60 different stimulants … which is why the[ conventional] paradigm doesn’t work.”
Low LDL Associated With Greater COVID-1 9 Severity
Interestingly, Saladino cites experiment demonstrating that low levels of LDL cholesterol are associated with greater COVID-1 9 severity. LDL and total cholesterol elevations were significantly lower in COVID-1 9 patients as to report to healthy themes. “To me, this is a really interesting[ observe] in two ways, ” Saladino says, adding 😛 TAGEND
“In’ The Carnivore Code, ’ I challenged the LDL-centric hypothesis of cardiovascular disease and I share a lot of information about how important LDL actually is in the immune plan. I think that’s exactly what we’re seeing in this study.
When your person is doing an immunologic thing, when your form is fighting a pathogen, it altogether obligates sense that the LDL would be a part of that, in either LDLs exhausted, or those who have lower LDL are more prone to infection.
This is something we encounter over and over, and there are even genetic conditions of very low LDL, specifically one called Smith-Lemli-Opitz syndrome involving a genetic polymorphism in an enzyme that meets cholesterol.
People with that illnes have very bad illness and they can be rescued by contribute them egg yolks. So these people are given cholesterol in the form of egg yolks, or they’re given supplemental cholesterol, and they do much better.
It’s pretty clear that cholesterol, which is packaged into this LDL lipoprotein particle, is intimately involved in the immune response. And so, in someone who is metabolically healthy, a higher LDL above 100 or 150, or even 200 mg/ dL might not be the shocking thing that we’ve all been taught it is, extremely if the HDL, the triglycerides, the triglyceride to glucose indicator, that glycemic variability, are all pointing toward metabolic state …
It’s about context. This LDL is a valuable immunologic speck and we can’t time get myopic, looking at LDL. We have to think about it in areas of all these other measures.”
Top Policy to Improve Your Metabolic Health
Considering the fact that your metabolic state establishes your COVID-1 9 probability, it would be a sound idea to implement policies that will improve your metabolic flexibility and insulin sensitivity. Saladino’s transcend recommendations for achieving that include 😛 TAGEND
1. Eliminate handled carbohydrates, carbohydrates, specks and vegetable oils — “I think that from a meat view, those are the key scourges that are really creating chao on our metabolism, ” he says. The worst perpetrator of them all is probably vegetable oils. “Polyunsaturated vegetable oils are highly oxidizable and particularly metabolically injury. So, begins with them, ” Saladino says.
For more information about this, witness “New Study Tells Why Chicken Is Killing You and Saturated Fat Is Your Friend, ” which peculiarities Saladino’s interview with science writer and columnist, Nina Teicholz. Saladino likewise recollects the mechanisms by which vegetable oils wreck health in greater detail in this interview, so be sure to listen to it in its entirety, or read through the transcript.
2. Eat animal foods — As noted in the paper, 12 “Immune Function and Micronutrient Requirements Change Over the Life Course, ” published in the periodical Nutrients, nutrient insufficiencies that can compromise immune function include vitamins, A, C, D, E, B2, B6, B12, folate, iron, selenium and zinc.
These vitamins are primarily found in animal foods, which is why shunning animal meat tends to lead to nutrient dearths. Even folate is found in organ fleshes in highly bioavailable form. “If you want to have a robust immune plan, you want to be metabolically healthy. You don’t want to be insulin-resistant and you need to have nutrient adequacy in your nutritions, ” Saladino says.
“How do you get nutrient suitability? You get these micronutrients from bioavailable informants in organ fleshes and in the muscle meat of animals.” If you cannot gut the idea of organ meat, consider using a desiccated parts add-on, such as those Saladino sells. 13
3. Time-restricted eating — Compressing the window of time in which you ingested down to six to eight hours a day, munching your last meal at least three hours before bedtime, is another very powerful strategy to improve your insulin sensitivity.
Eating a Varied, Real Food Diet Is Key
In short-lived, munching real meat, in a time-restricted window, is your surest gamble to beat insulin resistance. Likewise remember to give some consideration to your macronutrient ratios.
As explained by Saladino, while a low-fat, high-carb diet may increase your insulin resist, you’re at high risk for nutrient flaws in the long term, as so many of the most bioavailable vitamins and minerals are is located within animal-based fats.
“I think the sweetened recognise is gobbling an animal-based nutrition. Not alone swine for all people, but realizing that animal menus have been incorrectly smeared. They’re an integral part of the human diet, including part meats.
Also include some of the healthiest carbohydrates, the nonprocessed carbohydrates, into your diet sometimes, and don’t get either low-carb, high-fat all the time or low-fat, high-carb all the time. Having a mix, but having a robust amount of protein throughout … I think that’s a sugared recognize for most people.”
Low Glutathione May Increase COVID-1 9 Severity
Saladino also cites a recent hypothesis highlighting the potential role of glutathione in COVID-1 9. The working paper, 14 “Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Appearance of Death From Novel Coronavirus Infection( COVID-1 9 ): A Hypotheses Based on Literature Data and Own Observations, ” is written by a Russian medical doctor and Ph.D.
What he found was that the reactive-oxygen-species-to-glutathione ratio was able to predict the severity of COVID-1 9 and the patient’s outcome. When the patient had a low-spirited ROS-to-glutathione ratio, the patient had a very mild suit. The fever disappeared on the fourth epoch without any medication whatsoever.
When the ROS-to-glutathione ratio was high, individual patients developed breath emptines on the fourth period, knowledge significant fever, hoarseness, myalgia and lethargy persevering for 13 eras. A case with even higher ROS and lower shortened glutathione had critical cancer necessitating hospitalization for COVID-1 9-related pneumonia. Harmonizing to the author: 15
“Based on an extensive literature analysis and own sees, I proposed a hypothesis that glutathione deficiency is exactly the most plausible explanation for serious manifestation and fatality in COVID-1 9 infected patients.
The major risk factors established for severe COVID-1 9 infectious diseases and relative glutathione shortage found in COVID-1 9 fouled cases with moderate-to-severe illness have intersected me to two very important opinions 😛 TAGEND
( 1) oxidative stress contributes to hyper-inflammation of the lung leading to adverse disease outcomes such as acute respiratory distress syndrome, multiorgan failing and demise ;P TAGEND
( 2) inadequate antioxidant justification due to endogenous glutathione deficiency as a result of abridged biosynthesis and/ or increased depletion of GSH is the most probable cause of increased oxidative impairment of the lung, irrespective which of the factors aging, chronic disease comorbidity, smoking or some others were responsible for this deficit.
The hypothesis adds fiction revelations into the etiology and mechanisms responsible for serious manifestations of COVID-1 9 infectious diseases and vindicates predicting the possibility for effective management and prevention of the illness through glutathione recovering with N-acetylcysteine and shortened glutathione.”
Glutathione, Zinc and Selenium
As noted by Saladino, these meets too tie into the issue of zinc and its importance for proper immune purpose, as zinc helps mitigate the oxidative stress reaction. The question is, why do these people have such low-grade glutathione in the first place?
Saladino believes it’s probably due to underlying nutritional dearths such as glycine shortage, or oxidative stress caused by smoking, heavy metal toxicity, EMF exposure, munching lots of processed vegetable oils or insulin resist. Any of these could cause low glutathione.
To improve your glutathione, you need zinc, and zinc in combination with hydroxychloroquine( a zinc ionophore or zinc transporter) has been demonstrated effective in the treatment of COVID-1 9.
N-acetyl cysteine( NAC ), meanwhile, is a precursor of glutathione, and may protect against coagulation problems associated with COVID-1 9, as it antagonizes hypercoagulation and breaks down blood clots.
Selenium is also important, as some of the enzymes involved in glutathione production are selenium-dependent. Saladino quotes study establishing an association between regional selenium status and the severity of COVID-1 9 sequel actions in China. The lower the amount of selenium in the hair, the lower the cure rate was.
“Why is this? It’s probably because glutathione peroxidase and thioredoxin reductase are selenium- dependent enzymes, and these enzymes are intimately connected by ascertaining this antioxidant redox system, ” Saladino explains.
“So, what we’re seeing is this huge immunologic injury, this imbalance of the innate and adaptive immune method, we’re seeing insulin resistance, and we’re seeing spread oxidative damage, and all that stuff can probably be controlled with lifestyle. That’s the enormous takeaway.”
One of the best ways to increase glutathione, though, is molecular hydrogen. It is my absolute favorite as it does so selectively and will not increase glutathione unnecessarily if you don’t need it. You can view Tyler LeBaron’s excellent lecture on the details of how it does this in “How Molecular Hydrogen Can Help Your Immune System.”
More Information
We cover a lot of soil in this interview, far more than has been summarized here, so for more details, be sure to listen to the interrogation. Saladino is a wellspring of well-researched information. We also remembered 😛 TAGEND
The help of quercetin in lieu of hydroxychloroquine, either of which needs to be taken with zinc, at the earliest signs of symptoms.
The hazards of oxalates, is located within numerous plant foods and the benefits of a carnivore nutrition.
Joins between COVID-1 9 and pulmonary vasculitis — A brand-new hypothesis intimates SARS-CoV-2 strikes the endothelial cells that indication the blood vessels surrounding the lungs’ air sacs, or alveoli, making flowing leakage and blood clots. Harmonizing to Saladino, low-spirited glutathione may be at play here as well.
How you can improve your insulin predisposition in as little as nine periods by removing all fructose.
To learn more, be sure to visit his website, CarnivoreMD.com, and pick up a replica of “The Carnivore Code, ” now in its updated second copy. He also has a great podcast called “Fundamental Health.” On the social media stages, you can find him by searching for @ carnivoreMD.
“If those who are susceptible to COVID-1 9 due to insulin resistance and diabetes are able to use this as a wake-up call and change their metabolic state, they will change the quality of life for the entire time that they’re living, ” Saladino says.
“My dad is a perfect example of this. He’s 70 years old, a retired internist, and I’m going to get him a ceaseless glucose monitor. He’s not as metabolically health as he should be, but I’m encouraging him to improve his metabolic health.
And the charm of that might just be that if coronavirus is the impetus, if coronavirus is the trigger that he needs to change his metabolic health — to use a ongoing glucose monitor, to show himself his glycemic variability and understand how much risk that positions him at, or time to give him an indication that he’s a little insulin-resistant because he’s gobbling eat or vegetable oil, or not had enough nutrients.
If he makes the alter, he’s decreasing his peril of coronavirus, but he’s likewise decreasing his peril of seasonal flu, diabetic complications, coronary route cancer, hypertension and apoplexy. I entail, the directory goes on and on. That’s what you and I are about, and that’s what I think it’s all focused on.”
Read more: articles.mercola.com



Recent Comments