Alzheimer’s disease continues to be a leading cause of death in the U.S ., with 1 in 3 elders dying with Alzheimer’s or dementia — more than the count killed by breast and prostate cancers combined. 1
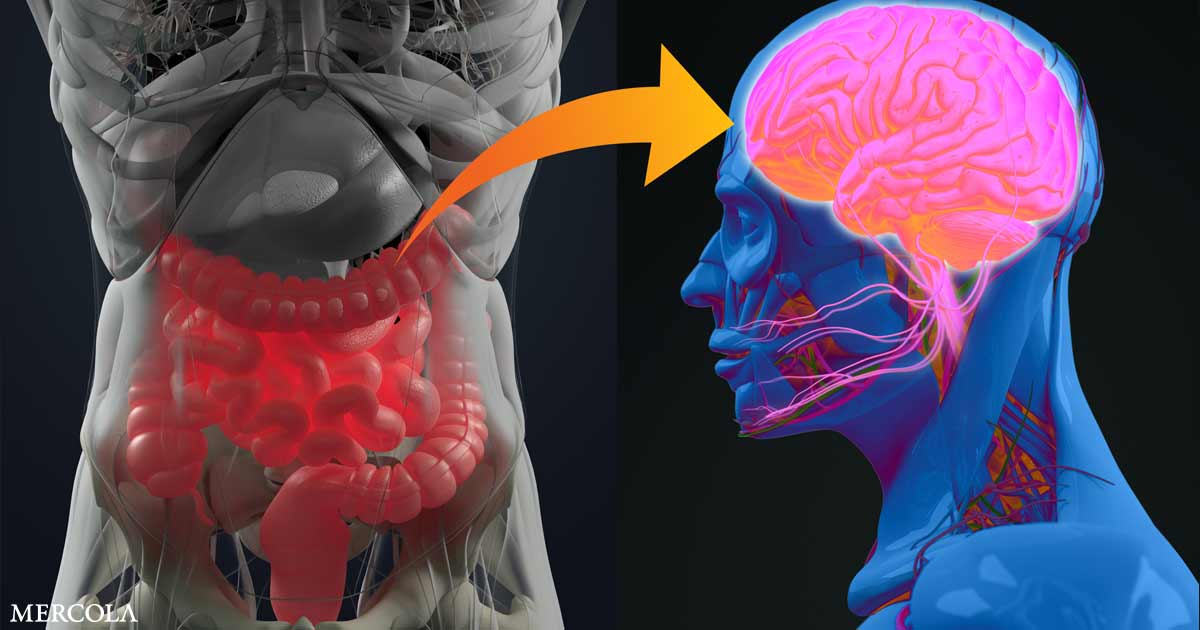
While a cure has remained elusive, the connection between brain health and gut microbiota has grown clearer, and research suggests that the bacteria in your entrails may influence brain functioning and can even promote neurodegeneration. 2
A team of Swiss and Italian researchers has made the linkage a gradation further, with investigate registering a the linkages between imbalanced bowel microbiota and the developing at amyloid plaques in the brain; 3 Alzheimer’s is characterized by an accumulation of beta-amyloid medals and neurofibrillary mess in the brain.
Proteins Produced by Gut Bacteria May Trigger Alzheimer’s
The study involved a cohort of 89 parties between 65 and 85 years of age. Some of them suffered from Alzheimer’s disease or other neurodegenerative diseases while others were healthful with no remembering problems.
The researchers squandered PET imaging to measure amyloid deposition in their brains, then valued markers of irritation and proteins produced by intestinal bacteria, such as lipopolysaccharides and short-chain fatty battery-acids, in their blood.
Lipopolysaccharides( LPSs) are dead bacteria or, more specifically, the cadre walls of dead bacteria. Your immune system analyses them as living bacteria and organizes immune protections against the realized aggressors. LPSs are pro-inflammatory and have been found in amyloid medals in the brains of Alzheimer’s cases. 4
The study revealed that high blood levels of LPSs and the short-chain fatty acids( SCFAs) acetate and valerate was made in association with big amyloid deposits in the psyche. Other SCFAs, namely butyrate, appeared to have a protective upshot; high levels of butyrate were associated with less amyloid.
Butyrate — an SCFA displayed when intestine bacteria fermenting fiber — triggers the secretion of brain-derived neurotrophic ingredient( BDNF ), 5 increased levels of which have been linked to Alzheimer’s disease.
“Our results are indisputable: Certain bacterial products of the intestinal microbiota are correlated with the quantity of amyloid plaques in the ability, ” justifies Moira Marizzoni, a study author with the Fatebenefratelli Center in Brescia, Italy. 6
Probiotic’ Cocktail’ May Act as an Early Preventative
The study represents a continuation of prior research by the team, which found that the nerve microbiota in beings with Alzheimer’s disease differs from those without the condition. In those with Alzheimer’s, microbial diversity is reduced, with certain bacteria being overrepresented and other microbes decreased.
“Furthermore, ” said neurologist Giovanni Frisoni, study author and director of the University Hospitals of Geneva( HUG) Memory Center in Switzerland, “we have also discovered community organizations between an inflammatory phenomenon identified in the blood, certain intestinal bacteria and Alzheimer’s disease; hence the hypothesis that we wanted to test now: Could inflammation in the blood be a mediator between the microbiota and the mentality? “7
With the connection growing stronger, the team is planning further investigate to discover which specific bacteria or groups of bacteria may be responsible for the effect, which could ultimately lead to a preventive treatment “cocktail.” Frisoni said in a news release :8
“Indeed, we must first identify the tightens of the concoction. Then, a neuroprotective impact could only be effective at a very early stage of the disease, with a view to prevention rather than therapy.
However, early diagnosis is still one of the main challenges in better management of neurodegenerative cankers, as protocols must be developed to identify high-risk individuals and treat them well before the figure of detectable symptoms.”
The Fasting Connection
One reason why fasting is so beneficial for neurodegenerative cankers such as Alzheimer’s is because it helps your body to cycle through autophagy and the rebuilding phase.
Autophagy is the process by which your mas cleanses out damaged organelles, encouraging proliferation of brand-new, health cadres, which relates to Alzheimer’s because the refolding process is one of several factors that need to work in order for your psyche to function.
Importantly, fasting activates autophagy, which is your body’s way of taking out the trash, and will likewise prompt the regeneration of stem cells. In our 2017 interrogation, Dr. Steven Gundry explained that this also may have a direct connection with LPSs, and giving your gut a respite from these pro-inflammatory proteins via fasting may be healing 😛 TAGEND
“We have an amazing repair system that goes to work when you’re fasting. Not the least of which is[ let] your intestine residual. It’s probably one of the smartest things that any of us can do — putting the wall of your gut at rest , not being able to assimilate nutrients , not having to deal with the constant inflow of lectins or virus. But I envisage most importantly, it renders[ your body] a chance to finally do some serious cleanup of your brain …
Alzheimer’s and Parkinson’s have a unifying cause, and that is the brain is attacking itself against recognized threat, a lot of which are LPSs. If you put your gut at rest and don’t have LPSs coming into your system, and the longer you can maintain that, realistically, the better off you are.
As Jason Fung would say, intermittent fasting is great; doing a qualified calorie-restricted diet is great, but it technically is so much easier to just stop eating … The second position of my revised food pyramid is ‘Don’t eat anything.'”
Probiotics Show Promise for Alzheimer’s
The effect of beneficial bacteria on brain health is well-established, be indicated in beings with Alzheimer’s disease. A 2016 study of 60 Alzheimer’s patients looked into the effect of probiotic augments on cognitive operate, with promising makes. 9 Those who drank milk containing probiotics knowledge significant improvements in cognitive function.
While average Mini-Mental State Examination( MMSE) scores increased among the probiotics group and the ascertain radical, which drink plain milk, had a decrease in scores.
The probiotics group also had helpful metabolic mutates, including lowered triglycerides, very low-density lipoprotein and C-reactive protein, a measure of inflammation, as well as shortened markers for insulin resistance.
The researchers showed the helpful metabolic varies may be responsible for the cognitive progress. Walter Lukiw, a professor at Louisiana State University who was not involved in the study, further explained to Medical News Today that your bowel and psyche are intricately connected: 10
“This is in line with some of our recent studies which indicate that the GI[ gastrointestinal] tract microbiome in Alzheimer’s is significantly altered in composition when compared to age-matched governs …
… and that both the GI tract and blood-brain barriers become significantly more leaky with aging, thus accepting GI tract microbial exudates( e.g. amyloids, lipopolysaccharides, endotoxins and small-scale non-coding RNAs) to access central nervous system compartments.”
Probiotics May Inhibit Neurodegeneration
Probiotics are thought to influence the central nervous system and behavior via the microbiota-gut-brain-axis, and researchers have suggested they may have both preventive and therapeutic possibilities for Alzheimer’s disease( AD) by modulating the inflammatory process and negating oxidative stress, among other mechanisms. 11 Writing in the open-access Impact Journal on Aging, investigates justified: 12
“It has been found that dysfunction in behavior and cognition is associated with GM[ nerve microbiota] dysbiosis. Activation of bowel irritation has been regarded as a possible pathogenic cofactor in cognitive impairment and dementia.
Moreover, the most distinctive differences in the GM of AD patients are weakened abundance of anti-inflammatory bacterial species( e.g. Bifidobacterium brevestrain A1) and strengthened abundance of pro-inflammatory flora phyla( e.g. Firmicutes and Bacteroidetes ).
And restoring GM homeostasis could slow down the progression of AD. Therefore, the GM has been proposed as a key player in the pathogenesis of AD and might be a brand-new possible therapeutic target for the prevention and treatment of AD.”
They attended a meta-analysis involving five studies and 297 themes, which revealed a significant improvement in cognition and a significant reduction in malondialdehyde and high-sensitivity C-reactive protein — inflammatory and oxidative biomarkers — in probiotic radicals compared to controls. 13
Research is still uncovering which bacteria are most beneficial, but the Bifidobacterium breve straining A1 may be of particular use in Alzheimer’s treatment. Using Alzheimer’s disease pattern mice, investigates were able to confirm that daily oral administered by B. breve A1 abbreviated the cognitive dysfunction normally induced by amyloid beta. 14
One of the mechanisms behind these protective impacts was found to be suppression of amyloid-beta-induced changes in gene expression in the hippocampus. In short, the bacterium had an ameliorating effect on amyloid-beta toxicity.
Still other study advocates gut microbiota may contribute to Alzheimer’s risk via variou boulevards, including by influencing aging, diabetes, sleep and circadian rhythm. 15
It’s also possible, researchers hypothesize, that decades of factors such as diet, stress, aging and genetics, combine to obstruct bowel permeability and the unity of the blood-brain barrier, standing the record of inflammatory operators and pathogens and generating an inflammatory response that provokes a neuroinflammatory response in the ability. 16
“There is mounting evidence that the bowel microbiota interacts with AD pathogenesis by disrupting neuroinflammation and metabolic homeostasis, ” they memorandum, adding that “the gut microbiota has get from being the leave organ to a potential leading player in the AD pathology.”1 7
Alzheimer’s Prevention Strategies
Optimizing your gut flora is a key strategy to preventing Alzheimer’s and a multitude of other chronic diseases. To do this, avoid processed foods, antibiotics and antibacterial produces, fluoridated and chlorinated sea, and be sure to eat traditionally fermented and cultured foods, along with taking a high-quality probiotic if needed.
Maintaining a healthy intestine is one of the healthy life parameters outlined by Dr. Dale Bredesen, professor of molecular and medical pharmacology at the University of California, Los Angeles School of Medicine, and columnist of “The End of Alzheimer’s: The First Program to Prevent and Reverse Cognitive Decline.”1 8P TAGEND
Bredesen’s ReCODE protocol evaluates 150 parts, including biochemistry, genetics and historic likeness, known to contribute to Alzheimer’s disease. This identifies your illnes subtype or combination of subtypes so an effective treatment protocol can be devised.
Time-restricted eating, or fasting, is another important strategy, as is reducing your intake of polyunsaturated fatty acids, too announced PUFAs, found in vegetable oils, edible petroleums, seed oils, trans fat and flower petroleums. A high-fat, moderate-protein, low net-carb ketogenic diet is ideal for preventing degeneration that can lead to Alzheimer’s, 19 and this will also help to nourish a healthful gut.
Overall , nurture your brain health is best done with a comprehensively healthful life-style. By leveraging 36 health life-style parameters, Bredesen was able to reverse Alzheimer’s in 9 out of 10 patients.
This included the use of exercising, ketogenic diet, optimizing vitamin D and other hormones, increasing sleep, musing, detoxification and eliminating gluten and processed food. For more details, you can download Bredesen’s full-text case paper online, which details the full planned. 20
Read more: articles.mercola.com




Recent Comments